TIPS Placement for Treatment of Budd-Chiari Syndrome
Ji Buethe, MD
Assistant Professor of Radiology
Interventional Radiology Center
The Johns Hopkins Hospital
1800 Orleans St.
Sheikh Zayed Tower, Suite 7203
Baltimore, MD21287
jbuethe1@jhmi.edu
Disclosures/Conflicts of Interest:
None
Introduction
Budd-Chiari syndrome (BCS) is defined as hepatic venous obstruction at the level of the hepatic veins, inferior vena cava (IVC), or right atrium1. Untreated symptomatic BCS has a high mortality rate, with up to 90% mortality within 3 years2. Management of patients with BCS depends on clinical and anatomic features, and includes diuretics, anticoagulation, thrombolysis, angioplasty, surgical portosystemic shunts, transjugular intrahepatic portosystemic shunt (TIPS) placement, and liver transplantation. TIPS in BCS can decompress congested hepatic vascular system by creating an alternative venous outflow tract3,4. While technically difficult, TIPS placement is a promising BCS treatment alternative to surgical portosystemic shunts or liver transplantation.
Case Report
A 64-year-old woman with a history of polycythemia vera complicated by BCS and cirrhosis presents with refractory ascites. A CT of the abdomen demonstrates cirrhotic appearance of the liver with stigmata of portal hypertension including splenomegaly, ascites, and splenorenal varices (Figure 1a). There is heterogeneous hypoenhancement peripherally in the liver with relative central and caudate hyperenhancement. Also seen is complete occlusion of hepatic veins and diminutive intrahepatic IVC. These finding are all in keeping with BCS. Additional findings include complete occlusion of the left portal vein, superior branch of the right portal vein, and splenic vein, as well as presence of prominent collateral veins in the porta hepatis and esophageal varices (Figure 1b).
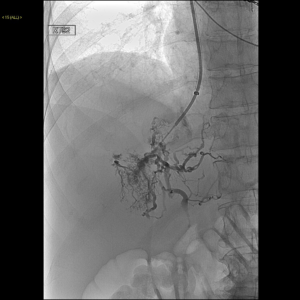
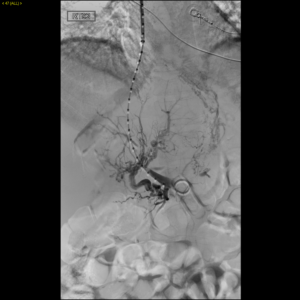
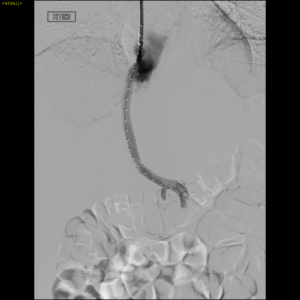
Laboratory tests revealed Child-Pugh score of 12, Model for End-Stage Liver Disease (MELD) score of 21, and Rotterdam class III (score 1.8). Given the patient’s extreme discomfort, pain, and dyspnea refractory to frequent large volume paracentesis, a decision was made to create a TIPS to relieve hepatic venous outflow obstruction despite the highly elevated MELD score. Under general anesthesia, the right internal jugular vein was accessed using a 5 French coaxial micropuncture introducer set and upsized to a 10 French sheath. Attempts to access the peripheral right hepatic vein revealed a short right hepatic vein remnant (Figure 2). Using landmarks on CT, the Rosch-Uchida needle (Rosch-Uchida Transjugular Liver Access Set, Cook) was advanced from the right hepatic vein stump into the portal vein. Venogram performed through the Rosch-Uchida sheath demonstrated spiderweb-like intrahepatic venous collaterals (Figure 3). After several attempts, portal vein was accessed. Portal venography was performed that showed hepatofugal flow, confirming portal hypertension (Figure 4). The hepatic parenchyma was dilated with an 8-mm diameter balloon, and a 10 mm x 8 cm (6 cm covered, 2 cm uncovered) Viatorr stent (W. L. Gore and Associates GmbH, Putzbrunn, Germany) was deployed across the liver parenchymal tract; placing the stent-graft into the main portal vein trunk. Given the long length of the parenchymal tract, a decision was made to extend the stent centrally using a 10 mm x 5 cm Viatorr stent (W. L. Gore and Associates GmbH, Putzbrunn, Germany) (Figure 5). Completion portography showed a widely patent shunt (Figure 6). The portosystemic pressure gradient decreased from 20 mmHg to 7 mmHg.
She had no post procedural complications and experienced complete resolution of pain and ascites within a week. She remains asymptomatic after 9 months of follow-up. Doppler US examination performed at 1, 3, and 6 months postprocedure confirmed a patent shunt.
Discussion
Since its first performance in the United States in 1990, TIPS has become an established therapeutic option for many complications of portal hypertension, such as bleeding varices, refractory ascites, hepatorenal syndrome, and hepatopulmonary syndrome5,6. More recently, TIPS has been utilized to treat more challenging cases such as portomesenteric venous thrombosis, polycystic liver disease, and BCS5-8.
Several reports suggest that TIPS placement can be successfully performed in patients with BCS 9-14. TIPS placement is an alternative therapy for relieving hepatic congestion, with lower mortality and morbidity than those associated with open surgical shunt creation. In one of the largest series on patients refractory to medical therapy or attempts at achieving recanalization, overall five-year survival after TIPS placement (84%) was similar to five-year survival from published reports of liver transplantation for BCS14. Transplant-free survival at one and five years after TIPS placement were 88% and 78%, respectively.
TIPS placement in BCS, particularly in the setting of complete thrombosis of all three hepatic veins, can be technically challenging. The difficulties encountered are primarily due to the absence of the hepatic vein and stiff liver parenchyma. Some cases may require a puncture from the remnant hepatic stump or direct IVC puncture (i.e. DIPS). In our case, we used the right hepatic vein stump as our starting point for transhepatic puncture into a portal vein. In conclusion, TIPS performed in properly selected patients can help improve BCS symptoms.
Figures
 Fig 1a. A contrast-enhanced CT of the abdomen demonstrates cirrhotic appearance of the liver with stigmata of portal hypertension including splenomegaly, ascites, and varices.
Fig 1a. A contrast-enhanced CT of the abdomen demonstrates cirrhotic appearance of the liver with stigmata of portal hypertension including splenomegaly, ascites, and varices.

Fig 1b. Reconstructed coronal maximum intensity projection (MIP) CT image of the abdomen demonstrates complete occlusion of the left portal vein, superior branch of the right portal vein, and splenic veins, as well as presence of prominent collateral veins in the porta hepatis and esophageal varices.
.
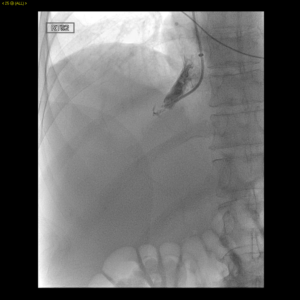
Fig 2. Right hepatic venogram demonstrates a short right hepatic vein remnant.
 /
/

- L. Janssen, J.C. Garcia-Pagan, E. Elias, et al. Budd-Chiari syndrome: a review by an expert panel. J Hepatol, 38 (2003), pp. 364-371
- Tavill AS, Wood EJ, Kreel L, Jones EA, Gregory M, Sherlock S SO. The Budd-Chiari syndrome: correlation between hepatic scintigraphy and the clinical, radiological, and pathological findings in nineteen cases of hepatic venous outflow obstruction.Gastroenterology. 1975;68(3):509.
- Valla DC. The diagnosis and management of the Budd-Chiari syndrome: consensus and controversies. Hepatology. 2003;38(4):793.
- Klein AS and Molmenti EP. Surgical treatment of Budd-Chiari syndrome. Liver Transpl. 2003;9(9):891
- Boyer T. Transjugular intrahepatic portosystemic shunt: current status. Gastroenterology 2003;124:1700–1710
- Bahramipour PF, Festa S, Biswal R, Wachsberg RH. Transjugular intrahepatic portosystemic shunt for the treatment of intractable ascites in a patient with polycystic liver disease. Cardiovasc Intervent Radiol 2000; 23:232–234
- LaBerge JM. Transjugular intrahepatic porosystemic shunt in portal hypertension. In: Han M, Park J, ed. Interventional radiology. Seoul, Korea: Ilchokak, 1999; 387–396
- Michl P, Bilzer M, Waggershauser T, et al. Successful treatment of chronic Budd-Chiari syndrome with a transjugular intrahepatic portosystemic shunt. J Hepatol 2000; 32:516–520
- Lopez RR Jr, Benner KG, Hall L, Rösch J, Pinson CW. Expandable venous stents for treatment of the Budd-Chiari syndrome. Gastroenterology. 1991;100(5 Pt 1):1435.
- Ochs A, Sellinger M, Haag K, et al. Transjugular intrahepatic portosystemic stent-shunt (TIPS) in the treatment of Budd-Chiari syndrome. J Hepatol. 1993;18(2):217.
- Ganger DR, Klapman JB, McDonald V, et al. Transjugular intrahepatic portosystemic shunt (TIPS) for Budd-Chiari syndrome or portal vein thrombosis: review of indications and problems. Am J Gastroenterol. 1999;94(3):603.
- PerellóA, García-Pagán JC, Gilabert R, et al. TIPS is a useful long-term derivative therapy for patients with Budd-Chiari syndrome uncontrolled by medical therapy. J Hepatology. 2002;35(1):132.
- Qi X, Yang M, Fan D, Han G. Transjugular intrahepatic portosystemic shunt in the treatment of Budd-Chiari syndrome: a critical review of literatures. Scand J Gastroenterol. 2013 Jul;48(7):771-84.
- Garcia-Pagán JC, Heydtmann M, Raffa S, et al. TIPS for Budd-Chiari syndrome: long-term results and prognostics factors in 124 patients. Budd-Chiari Syndrome-Transjugular Intrahepatic Portosystemic Shunt Group. Gastroenterology. 2008;135(3):808.